Launching November 7, 2014!
By: Adele Ryan McDowell, PhD
Sometimes a new book comes along that deserves a special shout out–this is one !
I am delighted to help spread the word about Adele McDowell’s new, powerful, and heart opening book.
I’ve known Adele for almost 18 years now, and she is the real deal: knowledgeable, compassionate, deeply empathetic, super-sensitive, and down-to-earth. She understands human suffering and human potential, the depths of pain and the triumphs of spirit, the reality of trauma and the tangible hold of hope.
The combination of her skill and personality make her the best person to approach and manage such a tender topic, and she does so with much heart and practical advice.
The book is filled with information and much needed explanations to one of the most heart-wrenching realities of human connection and loss. It is also filled with anecdotes, candid testimonies, and personal paths through grief and healing.
Read it!
Join the launching celebration on November 7 and be one of the first to own a copy!
Get it on November 7, 2014!
By: Adele Ryan McDowell, PhD

About the book:
Insightful, compelling, and compassionate, Making Peace with Suicide: A Book of Hope, Understanding, and Comfort takes a good hard look at the world-wide phenomena of suicide.
This book is designed for anyone who has lost a loved one to suicide and felt that sucker punch of grief; for anyone who is in pain, walking unsteadily, and considering suicide as an option; and for anyone who works with, guides, or counsels those feeling suicidal and/or suffering the profound grief from a suicidal loss.
Making Peace with Suicide includes stories of courage, vulnerability, and steadfastness from both the survivors of suicidal loss as well as the unique perspective of the formerly suicidal. It offers shared wisdom and coping strategies from those who have walked before you. It explores the factors leading to suicide and the reasons why some do and some don’t leave suicide notes.
Making Peace with Suicide sheds light on the phenomena of suicide vis-à-vis our teens, the military, new mothers, as an end-of-life choice, and asks if addiction is a form of slow suicide. It provides a seven-step healing process and opens the door to consider suicide and the soul, the heart lesson of suicide, and the energies of suicide.
If suicidality has impacted your life, Making Peace with Suicide is a must-read! You will be guided through the unknown territory, given insights to allow understanding, stories to help you heal, and ways to make peace with a heart wide-open. Making Peace with Suicide is good medicine for the body, mind, and soul.
Praise for Making Peace with Suicide
“Suicide is one of our most painful, difficult, confusing and wounding of human experiences. Dr. Adele McDowell addresses this topic with love and beauty. She non-judgmentally restores empathy, compassion and understanding. She courageously offers deep tending in a “place of primal pain.” And she is comprehensive, sharing the history, complexity, universality, and even positive dimensions of this mysterious act. Whether you are contemplating or have survived the attempt, lost someone to suicide, or counsel and help these populations, Adele McDowell’s Making Peace with Suicide will bring you hope, healing, compassion and understanding.”
–Edward Tick, PhD; Director, Soldier’s Heart; Author, War and the Soul and Warrior’s Return
“With sensitivity and compassion, Making Peace with Suicide explores the depth and breadth of suicide and offers insights and healing. This book is essential reading.”
–C. Norman Shealy, MD, PhD
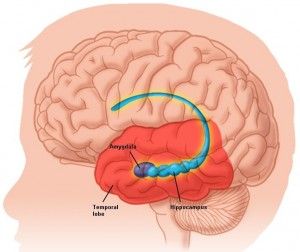
“No topic could be more timely than suicide. This remarkable book addresses people who have contemplated ending their lives as well as those who have to deal with the aftermath of those who succeeded. But it will also be invaluable to mental health workers and military chaplains, especially those who deal with young people who have been bullied and veterans with PTSD. For such a complex topic, Dr. McDowell’s writing style is reader-friendly and the stories she presents may well evoke tears. Her wise recommendations include teaching self-mastery techniques to help people cope with the stress of a success-oriented society. I have read many books on this sensitive topic, but none with the breadth and scope of Making Peace with Suicide.”
–Stanley Krippner, PhD; Co-author, Personal Mythology: The Psychology of Your Evolving Self and Haunted by Combat: Understanding PTSD in War Veterans
“Finally. A book that explains—in the simplest of terms, in a non-sensational, non-academic manner—the phenomenal, worldwide epidemic we call suicide. If you read one book on mental illness and how it affects our world, READ THIS ONE!”
–Ginny Sparrow, Editor, American Association of Suicidology
“Adele bravely and compassionately tackles a topic that many people avoid discussing—suicide. Yet in the understanding of it, the confusion and sense of loss is greatly eased. Making Peace with Suicide is rich with insight and healing methods all intended to help heal the void we feel when we lose a loved one to suicide. It’s also written for those who are suicidal to help them understand their pain and despair, and to let them know there is always help and there is always hope. I wish I had this book to read when my best friend took her life.”
–Carol Ritberger, PhD, author of Healing Happens with Your Help: Understanding the Hidden Meaning behind Illness
“This powerful book, written by a psychologist and former suicide-hotline responder, speaks to us all, about a present epidemic, surrounded by shame, taboo and secrets. Offering many personal stories, Adele helps the reader to find peace speaking to both those who believe they’re the only person who has ever felt this desperate and to the survivors whose lives are thrown into turmoil. This excellent book, full of useful resources, is essential for everybody who feels alone with their issues of life or death, bringing greater understanding, acceptance and comfort.
–Christine Page, MD, seminar leader & author of The Healing Power of the Sacred Woman
“As a minister/therapist for more than thirty years as well as a wife who lost her military husband to suicide, I have never found a more compassionate, effective book on suicide and its aftermath. This book serves many needs and highlights the myriad ways in which suicide changes one’s life direction. I cannot say strongly enough how powerful and helpful this book is.”
–Rev. Colleen E. Brown, Unity minister
“The loss of a loved one by any means is traumatic. When the loss is by suicide, in addition to the grief of the loss itself, survivors are often left riddled with guilt, anger, shame, and endless questioning, by both themselves and by others. In Making Peace with Suicide, Dr. McDowell gently and brilliantly weaves vital suicide survivor education with comforting and inspirational thoughts and quotes, all designed to direct the reader on a path of healing, resolution and peace. A must-read for anyone who has been touched by the tragedy of suicide and left to answer the question, ‘Why?’ ”
—Carole Brody Fleet, award-winning and bestselling author of Widows Wear Stilettos…; Happily Even After…; and When Bad Things Happen to Good Women…
“A subject such as this is never easy to digest. However, with Adele’s wisdom and guidance through her experience, this is a must read. We are in a new world now. Let Adele’s wisdom guide you with her insights for a new perspective on suicide.”
–Mona Delfino, author of The Sacred Language of the Human Body

Get Making Peace with Suicide on Amazon, November 7!











You must be logged in to post a comment.